Overview
Aortic valve regurgitation
Aortic valve regurgitation
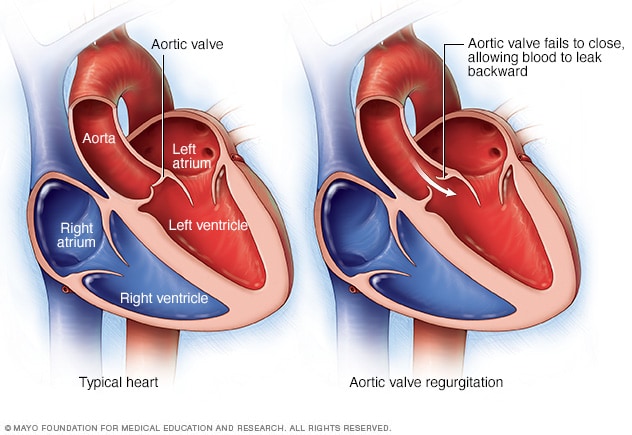
In aortic valve regurgitation, the aortic valve doesn't close properly, causing blood to flow backward from the body's main artery (aorta) into the lower left heart chamber (left ventricle).
Aortic valve regurgitation — or aortic regurgitation — is a condition that occurs when your heart's aortic valve doesn't close tightly. As a result, some of the blood pumped out of your heart's main pumping chamber (left ventricle) leaks backward.
The leakage may prevent your heart from efficiently pumping blood to the rest of your body. As a result, you may feel fatigued and short of breath.
Aortic valve regurgitation can develop suddenly or over decades. Once aortic valve regurgitation becomes severe, surgery is often required to repair or replace the aortic valve.
Symptoms
Most often, aortic valve regurgitation develops gradually. You may have no signs or symptoms for years. You may be unaware that you have the condition. However, sometimes aortic valve regurgitation occurs suddenly, usually as a result of an infection of the valve.
As aortic valve regurgitation worsens, signs and symptoms may include:
- Shortness of breath with exercise or when you lie down
- Fatigue and weakness, especially when you increase your activity level
- Heart murmur
- Irregular pulse (arrhythmia)
- Lightheadedness or fainting
- Chest pain (angina), discomfort or tightness, often increasing during exercise
- Sensations of a rapid, fluttering heartbeat (palpitations)
- Swollen ankles and feet
When to see a doctor
Contact your doctor right away if you have signs and symptoms of aortic valve regurgitation.
Sometimes the first signs of aortic valve regurgitation are related to heart failure. Make an appointment with your doctor if you have fatigue that doesn't get better with rest, shortness of breath, and swollen ankles and feet, which are common symptoms of heart failure.
Causes
Chambers and valves of the heart
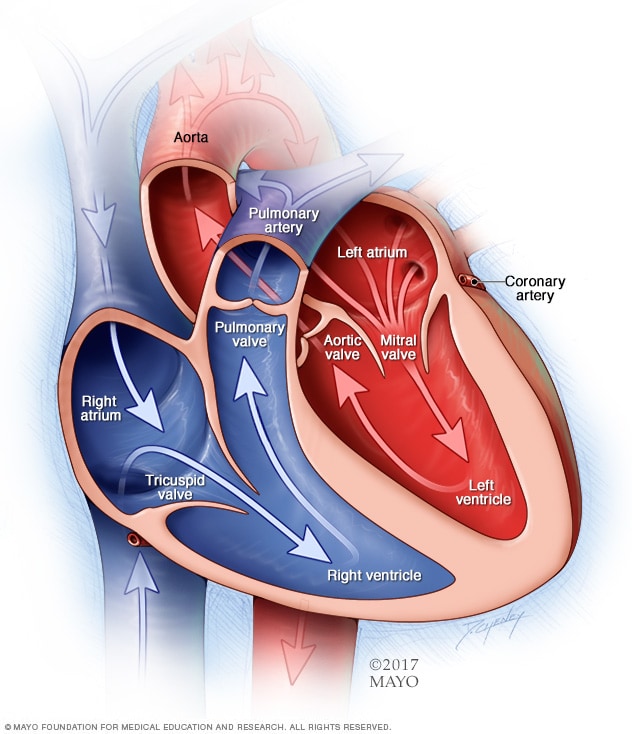
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
The aortic valve is one of four valves that control blood flow through the heart. It separates the heart's main pumping chamber (left ventricle) and the main artery that supplies oxygen-rich blood to your body (aorta). The valve has flaps (cusps or leaflets) that open and close once during each heartbeat.
In aortic valve regurgitation, the valve doesn't close properly, causing blood to leak back into the heart's main pumping chamber (left ventricle). As a result, the left ventricle holds more blood, possibly causing it to enlarge and thicken.
At first, the larger left ventricle helps maintain good blood flow with more force. But eventually these changes weaken the left ventricle — and your heart overall.
Aortic valve regurgitation usually occurs gradually, but it can develop suddenly when caused by a valve infection. Any condition that damages the aortic valve can cause regurgitation. However, you can develop aortic valve regurgitation without any known risk factors.
Causes of aortic valve regurgitation include:
-
Congenital heart valve disease. Some people are born with an aortic valve that has only two cusps (bicuspid valve) or fused cusps rather than the normal three separate cusps. Sometimes a valve may only have one cusp (unicuspid) or four cusps (quadricuspid), but this is less common.
These congenital heart defects put you at risk of developing aortic valve regurgitation at some time in your life. If you have a parent or sibling with a bicuspid valve, it increases the risk that you may have a bicuspid valve. However, you can have a bicuspid valve even if you don't have a family history of the defect.
- Narrowing of the aortic valve (aortic stenosis). Calcium deposits can build up on the aortic valve as you age, causing the aortic valve to stiffen and become narrow. This condition, called aortic stenosis, prevents the valve from opening, causing a blockage. Aortic stenosis may also prevent the valve from closing properly.
- Inflammation of the lining of the heart's chambers and valves (endocarditis). This life-threatening condition is usually caused by infection. It can damage the aortic valve.
- Rheumatic fever. Rheumatic fever is a complication of strep throat and was once a common childhood illness in the United States. It can cause the aortic valve to become stiff and narrow (stenosis), causing blood to leak. If you have an abnormal heart valve due to rheumatic fever, it's called rheumatic heart disease.
- Other diseases. Other rare conditions can enlarge the aorta and aortic valve and lead to regurgitation, including Marfan syndrome, a connective tissue disease. Some autoimmune conditions, such as lupus, also can lead to aortic valve regurgitation.
- Tear or injury of the body's main artery (aorta). A traumatic chest injury or aortic tear (dissection) may cause backward flow of blood through the aortic valve.
Risk factors
Things that make you more likely to develop aortic valve regurgitation include:
- Older age
- Certain heart conditions present at birth (congenital heart disease)
- History of infections that can affect the heart
- Certain conditions that can affect the heart, such as Marfan syndrome
- Other heart valve conditions, such as aortic valve stenosis
- High blood pressure
Complications
Possible complications of aortic valve regurgitation include:
- Fainting or feeling lightheaded
- Heart failure
- Infections that affect the heart, such as endocarditis
- Heart rhythm problems (arrhythmias)
- Death
Prevention
If you have any type of heart condition, see your doctor regularly so he or she can monitor you. If you have a parent, child, brother or sister with bicuspid aortic valve, you should have an echocardiogram to check for aortic valve regurgitation. Catching aortic valve regurgitation or another heart condition before it develops or in the early stages may make it more easily treatable.
Also, take steps to prevent conditions that can raise your risk of aortic valve regurgitation, including:
- Rheumatic fever. If you have a severe sore throat, see a doctor. Untreated strep throat can lead to rheumatic fever. Strep throat is easily treated with antibiotics.
- High blood pressure. Check your blood pressure regularly. Make sure it's well controlled to prevent aortic regurgitation.
Aug. 12, 2021